By Fabio Comana, MA, MS, NASM-CPT, CES, PES, NASM Faculty
That dreaded six-letter word that many of us know all too well. While we may be aware of some of the consequences of stress, the question that should be asked is what we are doing on a consistent basis to monitor and control these deleterious effects?
First off… what is stress? It is defined as a non-specific response by the body to any demand (stressor) that overcomes, or threatens to overcome, the body’s ability to maintain homeostasis (that state of equilibrium of the body’s internal biological mechanisms) (1,2). What this means is that regardless of the nature of the stressor (e.g., exercise, starvation, daily commute, work-related issues), the body perceives stress as a biological event and responds in essentially the same way. What differs is simply the magnitude of our response. This task is assigned to the brain that receives information about a stressor or any disruption to homeostasis and then initiates the appropriate ‘fight-or-flight’ response through the nervous system initially, prior to activating the hormonal system to share in this response (3). Keep in mind however, that imposing various levels of stress upon the body is quite natural and is actually critical to our survival as long as the body is afforded the opportunity for recovery between stressors to restore itself back to baseline (4).
Biological Design
The activation of our sympathetic nervous system (SNS) generates a more localized (i.e., location-specific), rapid-acting response which, in turn activates our hormonal response, generally considered a more generalized, slower-acting, but longer lasting response. In other words, the nervous system quickly stimulates a specific location like the adrenal gland to release necessary hormones like cortisol and epinephrine into systemic circulation in quantities related to the magnitude of the stress. These hormones exert their effect at multiple locations to preserve homeostasis and will remain in circulation until the stressor is removed. For example, epinephrine can simultaneously activate heart contractility, bronchodilation and peripheral arterial dilation in the exercising regions and remain in circulation until early recovery. These ‘fight-or-flight’ responses that affect our physiological systems are plentiful and collectively serve to ensure survival and success.
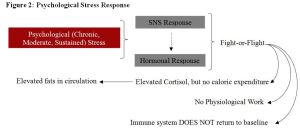
To gain a deeper insight into our biological stress response (i.e., our biological design), an example of how our ancestors survived may paint a clearer picture. The very nature of the stress during those times was very different to what we mostly experience today. Their primary stressors involved a fight for survival or to the death against a predator or aggressor (e.g., raiding party) and the nature of the stress was an intense, acute physiological response (Figure 1). However, after this brief, but stressful encounter, the body was afforded ample time to return to a state of calm or baseline. This ensured that each system (e.g., immune system) had time to complete any needed repair, recovery or replenishment. By contrast, our stress today generally involves lower-intensity, sustained psychological stressors that sometimes never go away, but simply compound themselves (Figure 2). For example, you might sleep through your alarm and wake up in a panic late for your meeting (stressor), skip breakfast (stressor), get caught in a slow commute (stressor), arrive late to your appointment where you needed to present a report (stressor), get reprimanded by your boss (stressor), finally make it to your office hoping to catch your breath, but receive a call that your child is sick and needs to be picked up from school (stressor) – sound familiar? This sustained stress denies our body that needed time to repair, recover and replenish.
Nonetheless, in either situation (ancestors v. present-day) the body activates its stress response in similar ways, albeit it at different intensities and while we are familiar with many responses (e.g., heart rate, blood pressure, mobilization of stored fats, increased sweat rates), we may not be aware of some of the others which do merit consideration. For example, under stress, epinephrine enhances our blood clotting ability by increasing platelet adhesiveness (4). By design, this may be needed to stop one from bleeding to death during a survival fight. Give thought now to constant elevated platelet adhesiveness on your cardiovascular health.
Ever wonder why you get dry mouth when nervous, why a dog may urinate when scared or why you need to run to the bathroom before a big race? Consider our need for survival – any events deemed unnecessary that expend energy (e.g., reproduction, growth, maintenance) during a period of intense stress are automatically shut down in order to provide the needed resources and energy to the necessary systems and locations to facilitate survival (e.g., muscles, skin for thermoregulation). The release of saliva, digestive enzymes and mucus in the mouth, stomach and upper GI that collectively facilitate chewing, digestion and absorption all shut down during stress as they consume energy. By contrast, smooth muscle contractility of the lower GI and bladder become activated to void unnecessary urine and fecal matter that may slow you down in the event you need to run to survive. Ever witness how an athlete suffers what appears to be a painful injury, yet manages to somehow play through it? Your fight-or-flight response will also temporarily decrease pain perception (analgesia) so you can sustain your fight-or-flight. Furthermore, systems involved in growth, repair, maintenance and reproduction are all temporarily inhibited under stress in order to provide the needed energy and resources elsewhere.
Table One: Stress Response Influence on Physiological Systems
Events Activated |
Events Inhibited |
Increased cardiopulmonary responsesIncreased vessel dilation in needed locationIncreased mobilization of fuelsIncreased blood clotting abilityIncreased large intestinal contractilityIncreased bladder contractilityIncreased immune function – short-termIncreased sweat rates |
Decreased salivary and digestive enzyme secretion, and digestionDecreased stomach/small intestinal contractilityDecreased pain perception (analgesia)Decreased growth, repair and maintenanceDecreased reproduction capacityImmune function – sustained long-term |
Sustained Stress
So what changes in the event of this sustained stress that many of us encounter daily in our lives? As we know, cortisol is a key hormone released from the adrenal gland in response to stress. Let’s first examine its role with blood sugar, especially during times when blood glucose levels become lowered. A primary role of cortisol is to avoid blood glucose depletion given how this fuel source is critical for optimal functionality and survival. Your brain may only weigh three to four pounds, but it may consume 25% of all your blood sugar in a 24-hour period. During periods of stress, blood sugar levels lower on account of increased muscle uptake or depleted liver glycogen. This activates cortisol release which regulates metabolism by reducing glucose utilization while favoring increases in both fat utilization and in gluconeogenesis, a term that defines the manufacturing of glucose from non-carbohydrates sources, like muscle protein (2,5). While fat utilization sounds great, the unfortunate reality in metabolism is that a carbohydrate by-product is needed for complete fat metabolism, but in the presence of elevated cortisol where carbohydrate breakdown is restricted, the body can attack available protein stores (primarily living muscle tissue, plus any ingested proteins) to make these byproducts and continue fat utilization. Imagine now the impact of elevated cortisol levels throughout your day.
From a biological standpoint, cortisol is noble in its intentions, yet ironically we cast it as a villain given its association with stress. For example, during an intense fight-or-flight response, carbohydrates serve as our primary fuel to perform physiological work. During recovery, it is the carbohydrate stores that need to be replenished, therefore cortisol stimulates Neuropeptide Y, a compound that triggers appetite. In this event, carbohydrates were consumed and energy reserves replenished. This consumption released insulin, which in turn lowered cortisol and appetite diminished. The consumption of carbohydrates also enhances serotonin release which can reduce anxiety associated with that stress (i.e., aid in recovery). However, under today’s psychological stress, we often experience the same response where some individuals crave carbohydrates when stressed and the calming effect that follows. Here unfortunately, the additional calories consumed are not replacing expended calories from physiological work, but simply adding to our total caloric intake.
Following below is a summary of some additional consequences associated with sustained, elevated levels of cortisol. Collectively the sustained effects of cortisol can result in less fat utilization; greater abdominal fat; reduced lean body mass; lowered metabolic rate; increased appetite and an increase in body composition. Essentially, not only does this deteriorate overall health and quality of life, but it may undo everything you are working so hard to accomplish with your clients.
Stress Management
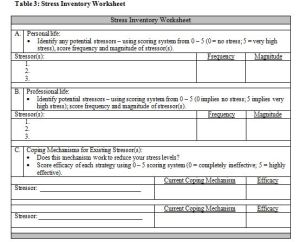
What are the key takeaways? Given the presence of stress in all our lives, any program for your clients that fails to inventory and address stress is incomplete and potentially ineffective. Take the time to complement your nutritional and exercise/activity efforts with a stress management program. Begin by first asking, listening and understanding stress levels in your client’s life. The worksheet presented below in Table 3 provides an example of a Stress Inventory Worksheet you might utilize. With an understanding, you can then effectively respond with strategies ideally suited to your client’s preferences and capabilities.
What stress-coping mechanism can you employ to help reduce your client’s stress levels? Many different techniques exist that demonstrate varying levels of success and while they should all be considered, select the one(s) most appropriate for your client(s) (7). Examples include:
- Deep Breathing (also known as paced breathing; belly, abdominal or diaphragmatic breathing):
- Find a place (physically or by clearing your mind) free of distractions.
- Close your eyes; and after a few normal breaths, draw in one long-slow breath through your nose engaging your diaphragm (include your chest – apical, if so desired).
- Pause momentarily, then slowly exhale through your mouth.
- Repeat for 30 – 60 seconds.
- Mindful Techniques:
- Start by repeating the breathing sequence, but now visualize relaxing scenes or visualize / repeat (slowly) any focus word or phrase that helps you relax.
- Practice in a place free of distractions 1 – 2 x per day for a minimum of 10 minutes each time.
- Variations of this technique include:
- Progressive mind relaxation – gradual intensification of the image, word or phrase.
- Mindful meditation.
- Yoga, Tai Chi or Qi Gong – including mind-body movements.
- Feldenkrais or guided imagery – super-slow (eyes closed) visualization inducing a deeper sense of mindfulness and mental imagery – often used to rehearse before movement.
- Body Sensation Awareness:
- Noticing subtle sensations (e.g., itching, tingling) without judgment – let them pass (progressive relaxation techniques).
- Progressive muscle relaxation – technique of visualizing tension release from muscles using sequential muscle contractions.
- Noticing emotions and feelings (e.g., anger, sadness) with judgment – accept them and progressively let them pass (diminish).
- Stored Energy Release:
- Stress can sometimes create muscle tension.
- For example, a gazelle under intense SNS activation that has eluded the interest of a predator proceeds to jump around after stress removal to release muscle tension. Similarly, humans also need physical sources for stress removal (e.g., exercise, punching).
- Reprioritization:
- Create opportunities to reprioritize matters – following a stressful event, spend time on an enjoyable activity or with person(s) who holds high priority in your life (e.g., hugging/playing with your kids).
- This helps prioritize and build perspective.
- Social Support:
- Studies examining primates and our ancestors demonstrated how females, following bouts of stress, resorted to affiliative behaviors such as grooming and hugging that offers a social calming effect (i.e., lowered blood pressure, cortisol levels).
- Research on oxytocin levels in female primates and human ancestors demonstrated more of a friend-and-befriend response rather than a fight-or-flight response, where they tend to their offspring and bond with one another when stressed (8, 9).
- For females especially, help plan and develop social support system that offers this same calming effect.
- Predictive Information:
- Awareness or anticipation of type, magnitude and duration of stress enables development of effective coping mechanisms.
- For example, planning ahead for a restaurant meal by reviewing the menu when trying to control caloric intake helps cope with the stress of making a rushed decision.
- Information however, must be relevant (i.e., tied to stressful event) and must be time-appropriate (e.g., information provided 3 weeks prior to, or one minute prior to ordering offers little help).
- Sense of Control:
- Creating impressions of or actually having control of a stressful situation can reduce stress.
- Low levels of control plus stress demands = poor stress response, whereas higher levels of control plus stress demands = better stress responses.
- With mild-to-moderate stress levels, increased control promotes self-efficacy.
- With high stress levels, one may benefit from less control to avoid extreme pressure, desperation or blame should they not succeed.
- Cognitive Flexibility:
- This involves developing the ability to remove stressors that you do control, but adapting to those stressors you cannot control. In essence, it helps one interpret things as always improving (i.e., positive outlook with glass half full).
- The Serenity Prayer by Reinhold Niebuhr, a 20th century Theologian helps summarize this strategy:
- “Grant me the serenity to accept the things I cannot change, the courage to change the things I can, and wisdom to know the difference.”
Closing Remarks
We often claim that stress kills, but a more appropriate interpretation is that it is our inability to recover from stress is actually our problem. Considering our biologically-designed stress response and how we, as a species, have deviated from that function to where our response is now negatively impacting our existence, rather than ensuring our survival, shouldn’t we pay more attention to these effects? Why invest our, and our client’s valuable time, efforts, expertise and energy into making change, only to watch it potentially dissipate because we neglected to give stress the attention it deserves? We can no longer afford to ignore stress management in our training philosophy for health, fitness and/or performance. It is time to expand our concept of training into wellness and to rethink our training practices – train smart, not just hard.
References:
- Seyle, H. (1978). The stress of life. New York, NY: McGraw-Hill.
- Kenney, W. L., Wilmore, J.H., and Costill, D.L., (2012). Physiology of Sport and Exercise (5th). Champaign, IL: Human Kinetics.
- McArdle, WD, Katch, FI, and Katch, VL. (2015). Exercise Physiology; Nutrition, Energy and Human Performance. Baltimore, MD: Wolter Kluwer Health – Lippincott, Williams & Wilkins.
- Sapolsky, RM. (2004). Why Zebras don’t get ulcers. New York, NY: Henry Holt and Company, LLC.
- Hoehn, K, Marieb. EN. (2010). Human Anatomy and Physiology. San Francisco, CA: Benjamin Cummings.
- Palacios, R, Sugawara, I (1982). Hydrocortisone abrogates proliferation of T-cells in autologous mixed lymphocyte reaction by rendering the interleukin-2 producer T-cells unresponsive to interleukin-1 and unable to synthesize the T-cell growth factor. Scandinavian Journal of Immunology, 15(1): 25–31.
- The Harvard Medical School (2014). Relaxation techniques: breath control helps quell errant stress response. Family Health Guide. www.health.harvard.edu (retrieved 09/14).
- Taylor, SE. (2008). From social psychology to neuroscience and back. In Levine, R, Rodrigues, A and Zelezny, L. (Eds.) Journeys in Social Psychology: Looking Back to Inspire the Future. New York, NY: Psychology Press
- Taylor, S E, Burklund, LJ, Eisenberger, NI, Lehman, BJ, Hilmert, CJ, and Lieberman, MD, (2008). Neural bases of moderation of cortisol stress responses by psychosocial resources. Journal of Personality and Social Psychology, 95(1):197–211.